Written by Jonathan E Aviv (Clinical Professor of Otolaryngology, Icahn School of Medicine at Mount Sinai, USA), Sujana Chandrasekhar (Clinical Professor of Otolaryngology, Zucker School of Medicine at Hofstra/Northwell, USA) and Byron Thomashow (Clinical Professor of Medicine, Columbia University Medical Center, USA)
All that is shortness of breath is not pulmonary. We have identified a cohort of 18 outpatients in a general otolaryngology practice in New York City who presented with persistent shortness of breath (SOB) despite normal pulmonary imaging. All patients had cough, fever and SOB between March 15 – May 15, 2020 during the height of the COVID-19 pandemic in New York City, with the SOB persisting for 4 – 12 weeks at the time of their presentation. 3/12 were positive for COVID-19 IgG antibodies, one of whom also tested positive with a nasal swab polymerase chain reaction (PCR) assay. Due to limited access, only 12 patients were able to obtain an antibody test and only 7 were able to get the PCR test. Of the 4 patients who had spirometry as part of their pulmonary investigation, the flow volume loop showed flattening of the inspiratory curve in all 4.
History revealed that the SOB was generally not waking these patients up at night nor was it affecting their exercise tolerance. Indeed, they often reported feeling breathing difficulties after their activity. Talking, shouting, singing, and odors typically brought on the SOB.
On physical exam of the larynx with awake video transnasal flexible laryngoscopy, all patients demonstrated that their vocal folds were not moving in normal synch with their breathing, that is, they were closing more than 50% of their glottic airway during quiet respiration when they should be opening. This abnormal vocal fold adduction could also be elicited by having the patient say the 5-word sentence “we see three green trees” and observing the vocal folds slowly closing afterwards for as long as 9 seconds. We believe that the persistent vocal fold adduction gave the patients their SOB. The flattening of the inspiratory curve on spirometry corroborated the laryngeal exam findings. This is different than laryngospasm where the vocal folds suddenly slam shut for prolonged periods of time and gives a different symptom profile.
This vocal fold dysfunction, or paradoxical vocal fold movement disorder [1], is a vagal neuropathy, often occurring after a viral illness. One of the reasons it has traditionally been difficult to make the diagnosis of post viral vagal neuropathy is that most people are unable to recall that they had a viral illness, especially if the inciting event happened years ago. In the time of coronavirus, patients seem to be paying much more attention to when they began to feel ill.
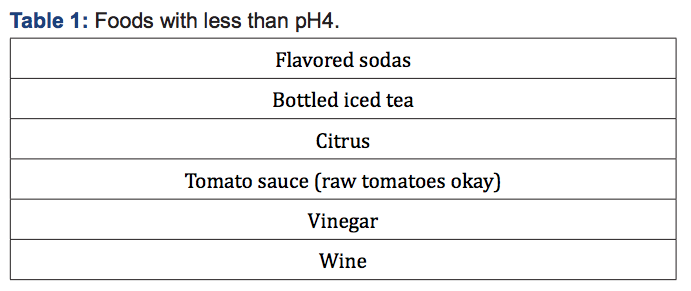
Our cohort was treated successfully with a combination of physical therapy – respiratory retraining – and diet modification techniques. The handful of foods and beverages less than pH4 (Table 1) tend to aggravate the breathing issues so we recommended that they be avoided.
We feel that in a time of understandably great emphasis on serial CT scans of the chest to evaluate patients with persistent shortness of breath, offering this other, emerging diagnostic possibility to account for such symptoms may be helpful to the clinician. In patients with persistent SOB, with or without cough, where the pulmonary imaging is unremarkable whether or not they tested positive for, or have antibodies to, Covid-19, but certainly with positive testing, one should consider both a spirometry and an otolaryngology evaluation. This symptom complex may be due to a virus-related cranial neuropathy which can be readily identified with office laryngoscopic evaluation and then treated, with restoration of premorbid functionality.
